Alo Yeditepe
Alo Yeditepe
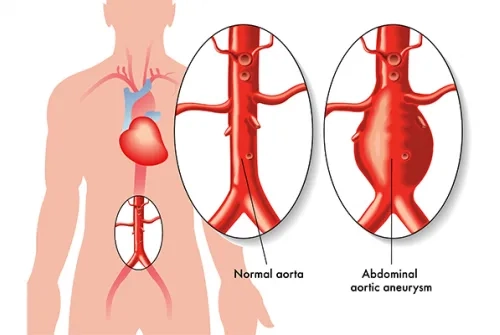
What is an Aortic Aneurysm? How is it treated?
What is Aortic Aneurysm?
"Aortic aneurysm is defined as a condition where the main artery called the aorta expands beyond a certain diameter due to various reasons. Particularly, the absence of significant complaints in the patient until it reaches an advanced stage, combined with the fact that delays can pose a life-threatening risk, underscores the importance of raising awareness about aortic aneurysm."
What Causes Aortic Aneurysm?
The diameter of the aorta, the main artery that carries blood from the heart, is typically 28-32 millimeters for individuals of average height and weight. When this diameter increases beyond a certain point due to various reasons, it's referred to as "dilatation," and when the aorta becomes excessively wide, leading to a risk of tearing or separating into layers, it's defined as an "aortic aneurysm." The aorta, responsible for carrying oxygenated blood to all our organs, maintains blood pressure within it. It's important to note that with each heartbeat, blood pressure rises and partially drops when the heart relaxes and the aortic valve closes. The blood pressure measured in the arm reflects this pressure. To withstand this pressure, there are micro-level, evenly arranged, flexible, and strong connective tissue fibers in the aortic wall. Thanks to these fibers, the aortic wall can stretch to adapt to changes in blood pressure.
In some diseases that affect connective tissues like atherosclerosis, the function of regenerating fibers gradually diminishes with age. However, the deterioration continues. In some cases, there may also be cracks in the fibers during their production phase. Under the influence of blood pressure inside the aortic wall, the weakened areas of the aortic wall begin to thin and expand.
It is quite common for individuals with bicuspid aortic valves (two leaflets instead of the usual three) to develop aortic aneurysms. The valve itself usually does not cause problems until middle age. In a minority of patients, it may lead to stenosis (narrowing) or regurgitation (the valve not closing properly, allowing blood to flow back), often occurring in conjunction with an aortic aneurysm. Pathological examination in these patients also reveals weakness and fractures in the connective tissue fibers of the aortic wall.
According to the laws of physics, the wall tension, which increases proportionally with the square of the aortic radius, can lead to outward ruptures (rupture) or the separation of the layers constituting the aortic wall (dissection) in the weakened and thinned aortic wall.
In the ascending aorta, which starts with the aortic valve and extends to the region where the arteries leading to the arms and brain are located, the upper limit for an acceptable expansion is 50 millimeters. Beyond this diameter, each millimeter increase in diameter significantly increases the likelihood of rupture or dissection. Since the ascending aorta, up to this diameter, has no immediate neighbors, increased diameter doesn't typically cause compression symptoms, meaning the patient may not experience any symptoms. Up to this stage, the diagnosis can be easily made through cardiology assessments like echocardiography or chest X-rays, which show the expanded portion of the aorta.
What Are the Symptoms of Aortic Aneurysm?
If an aneurysm reaches 7-8 centimeters in size or puts pressure on surrounding organs, symptoms such as difficulty swallowing or shortness of breath may occur. Sometimes, the development of aortic insufficiency, where a significant amount of blood flows backward with each heartbeat, can lead to a sensation that one's "head" is shaking with each heartbeat, a symptom known as 'Musset's sign,' named after the famous French writer Alfred de Musset, who experienced the same symptoms with this condition.
If an aneurysm forms in more advanced parts of the aorta, such as in the next section called the Arch of the Aorta, where the arteries leading to the arms and brain exit, it can cause shortness of breath and difficulty swallowing by pressing on the adjacent trachea and esophagus. Furthermore, in the abdomen, internal organ compression symptoms can occur. Patients may report feeling their pulse in their abdomen or even claim that their abdomen moves with each pulse beat. When we gently place our hands on the patient's abdomen, especially in a thin individual, we can often easily feel a ballooned segment of the aorta that has grown like a balloon and pulsates with each heartbeat. If local expansions affecting arteries responsible for feeding internal organs occur within the aneurysm sac, the formation of clots within this sac, embolisms caused by these clots traveling to organs or legs, dissection, or blockage of blood flow to organs due to the aneurysm, known as organ infarctions, can lead to fatal complications.
The ascending aorta, which is adjacent to the heart within the pericardial sac, is an organ that is responsible for pumping blood to the heart. Rupture of this aorta results in rapid filling of the pericardial sac with blood, a condition called cardiac tamponade, which can lead to death within a few minutes. In this region of the aorta, there is no tissue that can prevent bleeding, and there is no external pressure. Therefore, this is the most common complication area for aneurysms and results in death. Connective tissue diseases and Bicuspid Aortic diseases are considered the main causes of aneurysms in this region. The Arch of the Aorta, where an aneurysm may occur next, is a region where two-thirds of the surroundings consist of dense muscle, bone, and connective tissue. Since the aorta itself also has a relatively thicker outer layer, the probability of survival and reaching the hospital during rupture is higher. However, this region is further from the chest or abdominal cavities. When it opens into these cavities, such as the chest or abdominal aorta, it can result in death within minutes. Usually, severe pain is felt at the site of rupture, and in cases of significant blood loss, shock may occur in the patient. As we move away from the heart, atherosclerosis, also known as hardening of the arteries, becomes the primary cause of aneurysm formation. These patients are typically significantly older than those with ascending aortic aneurysms and often have coexisting conditions such as coronary artery disease or atherosclerotic diseases of the brain arteries.
In the complications of aortic aneurysm rupture or dissection, approximately 70% of patients lose their lives during the event. More than half of the surviving patients can be lost within the first 2 hours if they are not urgently operated on. Both conditions require emergency surgery, and the risks of complications and mortality for surgeries performed at this stage are much higher compared to surgeries performed "before the aortic tissue is damaged."
When Are Patients with Aortic Aneurysm Operated On?
Aortic aneurysms can sometimes be diagnosed incidentally during medical evaluations for other complaints, conducted by specialties other than cardiology or cardiovascular surgery. For example, a computed tomography scan taken as a result of a lung infection can clearly show which part of the aorta has expanded and to what extent. Sometimes, when cardiac sounds are listened to by a physician from another specialty, a murmur caused by stenosis or insufficiency of the aortic valve can be heard. When the patient is referred to cardiology, a diagnosis of valve disease or an aneurysm, if present, can be easily made. After diagnosis, patients with an aorta that has expanded but is still within surgical limits, meaning the diameter of the ascending aorta is less than 50 mm, are monitored with echocardiography or preferably computed tomography scans at intervals of 3 to 6 months. When the diameter reaches this threshold, surgery is performed without further delay. During follow-ups, if there is an increase of more than 3 mm within a 6-month interval, the patient is scheduled for surgery before the diameter reaches 50 mm.
In conditions with certain connective tissue disorders like Marfan syndrome, Ehlers-Danlos syndrome, or annuloaortic ectasia, aneurysms of the aorta and other arteries can develop at much younger ages. In such diseases, dissection and rupture occur at earlier ages, and as a result, they are operated on before reaching these diameters because the aortic tissue is much weaker in these cases.
Can Aortic Aneurysms Occur at a Young Age?
The most significant problems seen at a young age are aneurysms associated with genetic connective tissue disorders. After the age of 30-35, aortic aneurysms related to bicuspid aortic valves come to the forefront. In aneurysms seen in older age, aortic valve diseases are sometimes responsible, and most often, it is caused by a condition called atherosclerosis, which is artery hardening.
What Factors Affect the Success of Surgery?
In surgeries performed before the condition known as dissection occurs, that is, before the layers of the aorta separate or tear, much more successful results can be achieved. However, especially in these major surgeries that can pose serious life risks, highly complex surgical techniques are used, so experience is of great importance. In addition, another important point to achieve successful results is to act early.
What Methods Are Used in Aortic Aneurysm Surgery?
With the advancement of technology, aneurysms in the chest aorta and abdominal aorta can now be repaired using endovascular procedures, which involve placing grafts wrapped around a stent inside the artery through small surgical incisions made in the groin area. Calling this a traditional surgery may not be accurate; the patient's skin incisions are only a few centimeters in size and are made in the groin area. Over the past 15-20 years, an increasing number of aortic aneurysms in the chest and abdomen can be treated with this new technique called Endovascular Aortic Repair (EVAR). Nowadays, patients with anatomical features unsuitable for EVAR, especially those with "only a small portion" of the aneurysm suitable for treatment, still undergo traditional open surgeries.
For aortic aneurysms located close to the heart, EVAR studies are ongoing. However, due to the proximity of the aortic valve and the coronary arteries that originate just above it, traditional open surgeries are still considered the gold standard. Similarly, surgeries for Arch Aorta, which involve the exit points of the arm and brain arteries, can still be repaired using open surgical methods. The limited application of custom-made grafts (Custom grafts) with the EVAR method on humans, which is still under development, has led to cautious approaches to this technique.
What Precautions Should Be Taken to Prevent Aortic Aneurysm?
First of all, routine check-ups are important at every age to prevent heart diseases;
Children's Check-ups:
For this reason, every child should be evaluated by a specialist in terms of the cardiovascular system, and regular follow-ups should be maintained throughout the growth period. In case any abnormality is detected in the cardiovascular system, a pediatric cardiologist should be consulted.
Control of Adolescents:
Between the ages of 20-35, it is a relatively safe period for cardiovascular diseases in humans. However, syndromes associated with connective tissue anomalies are most commonly seen in this age group. In such cases, symptoms related to the disease may include visual disturbances, joint and spinal deformities, elongated arms and legs, and palate shape abnormalities. These patients often exhibit excessive flexibility in their finger joints. In such cases, it is essential to consult a cardiologist without delay.
Familial Heart Disease Control:
"The presence of a family history of heart disease is also highly significant in aortic aneurysms. In families where there is a history of 'early and sudden death,' even if the cause is unknown, it should always be kept in mind that individuals may be 'potential heart patients,' and it is advisable for women to start cardiology check-ups at the age of 40 and men at the age of 35."
Check-ups for Healthy Individuals:
Even individuals without any health problems and without a family history of heart disease should undergo periodic examinations and tests for the cardiovascular system starting at the age of 45 for women and 40 for men. This is a proactive measure for maintaining good health.
About
Faculty and Year of Graduation:
Istanbul Faculty of Medicine, 1988
”
See Also
- What is a Bypass? How is Bypass Surgery Performed?
- Surgical Treatment of Heart Valve Diseases
- He Went to the Hospital with Leg Pain, Discovered His Carotid Artery Was 95% Blocked
- Does an Aortic Aneurysm Show Symptoms ?
- Aortic Aneurysm
- You Can Be Protected from Varicose Veins During Pregnancy
- Drug Treatment is Priority Leg Vein Obstructions
- Cardiovascular Diseases
- Pain in the Legs May Be a Sign of Vascular Congestion
- Which Diseases Can Swelling in the Legs Indicate?
- Stay Away from Depression and Protect Your Heart!
- Do Not Let Varicose Veins Be Your Nightmare During Pregnancy!
- Frequently Asked Questions About Varicose Vein
Alo Yeditepe