Alo Yeditepe
Alo Yeditepe
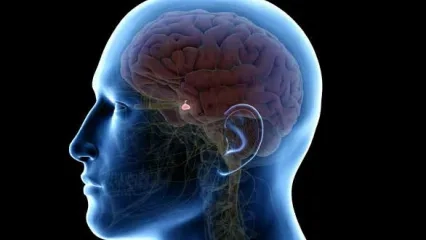
Treatment of Pituitary Adenomas
Radiotherapy has been used in the treatment of pituitary adenomas for many years. Radiotherapy is applied to tumors with atypical or carcinoma histopathological diagnosis if the tumor cannot be completely removed after maximum safe resection, the tumor continues to grow again after surgery and/or excessive hormone secretion.
The main goal of radiotherapy is to reduce abnormal hormone values to normal levels and to control tumor growth. Postoperative radiotherapy is recommended to prevent this, as the tumor is likely to grow again if the tumor cannot be completely removed. In this group of patients, treatment can be done in the first six months after the operation as well as later. Radiotherapy can be performed if growth is detected in the tumor tissue that cannot be removed by examinations after surgery.
What Types of Radiotherapy Are Used in Pituitary Adenomas?
Radiotherapy can be applied to these tumors in two different techniques.
If the tumor is very close to critical organs and it is difficult to protect intact tissues while irradiating the tumor, the planned radiation dose (45-54 Gy) is divided into 25-30 days and given 5 days a week. These treatment techniques are described as three-dimensional conformal therapy (3D conformal) or intensity-adjusted radiotherapy (IMRT).
If critical organs are far away or can be preserved, treatment is performed by dividing the total equivalent dose to be given into days 1-5 and applying it on consecutive days.These treatment techniques (Stereotactic radiosurgery and radiotherapy) are called SRS or SRT. The aim here is to provide maximum protection of intact tissues while controlling the tumor by giving a very high dose to the tumor in a short time.
Gamma Knife is a frame-based system that uses 192 conically arranged radio-active cobalt-60 sources to create targeted multi-focus beam shots.
A fixed frame or frameless mask can be used in a LINAC-based SRS system, and treatment is usually performed using multiple dynamic conformal arcs (VMAT) or intensity-adjusted radiation therapy (IMRT) to focus the dose on the middle of the target. CyberKnife ™ is a robotic-based radiotherapy system with a robotic image-guided system and mobile linear accelerator that allows the use of a frameless mask with SRS. Each radiotherapy system has advantages and disadvantages.
How is Radiotherapy Administered?
When planning radiation therapy for pituitary adenomas, the main goal is to minimize the dose to critical structures. In this region, the optic nerves, chiasm, brain stem, pituitary stem, and pituitary itself are the organs at risk. It is important to determine the organs at risk (oar) correctly because the pituitary is close to many critical structures.
Reducing the dose at which the normal pituitary gland is affected may prevent radiation-related neuroendocrine problems. Classically, SRS is not recommended for tumors less than 3 mm from the optic chiasm. Because it is very difficult to protect the optic nerves while giving an effective dose for the tumor. When dose constraints cannot be achieved for tumors close to the optic nerves, the planned dose may be fractionated.
What Are the Side Effects of Radiotherapy in the Treatment of Pituitary Adenoma?
Fractional radiation therapy and SRS are important treatment options for patients with pituitary adenoma. During fractional radiation therapy, patients may experience complaints such as temporary hair loss, skin erythema, fatigue, and headache. However, more serious side effects such as vision loss or other cranial nerve deficits are rare. With frame-based SRS, acute side effects may include numbness, tenderness, and bleeding at frame pin sites. A possible headache and fatigue may be seen in the treatment of SRS and SRT.
Long-term side effects include hypopituitarism, optic neuropathy, other cranial neuropathies of the cavernous sinus, radiation necrosis, neurocognitive effects, vascular complications, and secondary malignancies. Hypopituitarism is the most common long-term side effect and is estimated to occur in approximately half of the patients receiving radiation therapy.
This content was prepared by Yeditepe University Hospitals Medical Editorial Board.
”
See Also
- What is Hypoglycemia?
- Did You Know That Our Bodies are Managed by Hormones?
- Misconceptions About Hypertension
- What is Hypertension?
- Chronic Pelvic Pain
- What is Polycystic Ovary Syndrome/PCOS?
- The Hidden Problem Seen in One out of Every 10 Women: HIRSUTISM
- Persistent Headache May Be a Sign of Tumor
- The Purpose of Pituitary Diseases is to Avoid Waste of Time with the Right Treatment
- Pelvic Floor Muscles Should Be Addressed with a Multidisciplinary Approach
- Protect Children From Sports That Will Knock Their Head
- Polycystic Ovary Syndrome Can Occur If the Bacteria in the Gut Are Not Functioning Well
- Doctor Support for the Ban on Heading by Children
- Head Trauma Can Cause Permanent Damage
- Diabetes Mellitus and its Treatment
- Surgical Treatment of Pituitary Diseases
- Pituitary Clinic | FAQs
- What are Pituitary Diseases?
- What is the Pituitary Gland, What are its Functions?
- What is Hirsutism?
- Hirsutism Clinic / FAQs
- Treatment Success in Brain Tumors Also Depends on the Family
Alo Yeditepe