Alo Yeditepe
Alo Yeditepe
Radioembolization in Liver Tumor Treatment
Although surgical treatment has a very important place in the treatment of liver tumors, which have increased in frequency in recent years, only a small portion of patients, such as 20 percent, have the opportunity to undergo surgery. Nuclear Medicine Specialist Prof. Dr. Nalan Alan SELÇUK explains that the radioembolization method is used in liver tumors that do not have a surgical chance. Dr. SELÇUK and Interventional Radiology Specialist Assoc. Dr. Melih TOPÇUOĞLU pointed out that liver tumors have been increasing in our country in recent years and gave information about radioembolization treatment, which helps increase the life expectancy of patients.
What is TransArterial RadioEmbolization?
The use of the TARE (TransArterial RadioEmbolization) method, which is used in cases where liver tumors and different organ cancers metastasize to the liver, is increasing. Nuclear Medicine Specialist Prof. Dr. Nalan Alan SELÇUK said that the application requires an interdisciplinary approach. Dr. SELÇUK and Interventional Radiology Specialist Assoc. Dr. Melih TOPÇUOĞLU explained that this method is used especially in patients who do not have the opportunity for surgery and successful results are achieved.
Yeditepe University Koşuyolu Hospital Nuclear Medicine Specialist Prof.Dr. Nalan Alan SELÇUK pointed out that the frequency of liver cancer has increased in our country as well as in the whole world in recent years, due to the increase in diagnostic possibilities and environmental factors. Dr. SELÇUK pointed out that the importance of radioembolization treatment has therefore increased. Regarding this treatment, which is carried out by administering radioactive substances to the body, Prof. Dr. N. Alan SELÇUK said, “We apply radioembolization especially in hepatocellular cancer of the liver, which we call HCC or cholangio cancer. "We also apply radioembolization treatment in colon cancer and liver metastases of breast and neuroendocrine tumors," She said.
‘’As Liver Tumors Increase, the Need for RadioEmbolization Application Increases”
Interventional Radiology Specialist Assoc. Dr. Melih TOPÇUOĞLU also explained that in patients who do not have a chance for surgical treatment, the patient can become suitable for surgery after radioembolization treatment. In this context, Dr. TOPÇUOĞLU touched upon the importance of radioembolization treatment in liver tumors. Dr. TOPÇUOĞLU stated that radioembolization is one of the interventional radiological treatment methods and said that the need is increasing day by day as the detectability of liver tumors increases.
Dr. TOPÇUOĞLU stated that only a small portion of these patients can be treated surgically and said, “We can intervene in patients who do not have the option of surgery. All over the world, these treatments have been performed with increasing frequency for approximately 30 years. When we apply it to patients who do not have surgery, we can shrink the tumors of those patients and make them suitable for surgery. In some patients, we can completely eliminate tumors and contribute to prolonging their lives. "There are many options available," he said.
“It is important for the application of TARE that the tumor is limited to the liver in patients”
Prof. Dr. N. Alan SELÇUK stated that local treatments include the TARE treatment method, which is applied in cooperation with nuclear medicine and interventional radiology, and gave the following information about the situations in which they use the treatment: “In patients who have lost their chance for surgery and have multiple tumors within the liver, tumors can be reduced or reduced with the TARE method.” can disappear completely. However, it is important for the application that the tumor is localized to the liver, that is, it is limited only to the liver. "If these tumors originating from the liver or metastasized affect the patient's quality of life, or if the liver tumor determines the patient's prognosis, that is, the progression of the disease, we activate this treatment."
How is RadioEmbolization Treatment Done?
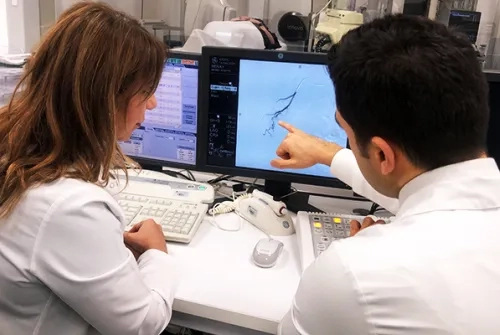
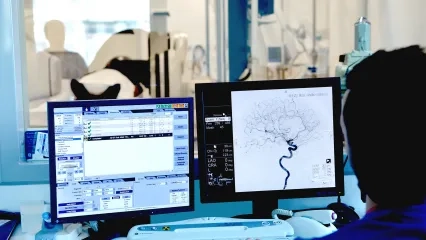
Explaining that they also use radioembolization treatment in colon cancer and liver metastases of breast and neuroendocrine tumors, Prof. Dr. Nalan Alan SELÇUK gave the following information about the application: “Radioembolization, carried out together with interventional radiology, is a two-step method. First, a rehearsal is made and angiography of the liver is performed. "We find the vein that feeds the tumor and calculate the dose of radioactive material to be administered to the patient," she said.
Are the Radiation Doses and Amounts Received by Patients Different in RadioEmbolization Treatment?
Reminding that a rehearsal was made before the treatment, Nuclear Medicine Specialist Prof. Dr. Nalan Alan SELÇUK said that the purpose of the rehearsal is to predict whether the patient will benefit from this treatment and to determine the amount of radiation given to destroy the tumor in the appropriate patient. Underlining that this treatment is personalized, Prof. Dr. SELÇUK explained: “Each patient's vascular structure is unique. For this reason, mapping the patient's vascular structure is important for detecting leaks of radioactive substances to be administered through treatment. In some patients, it appears that the vessels feeding the liver also feed other organs. In such a case, the radioactive substance you give without rehearsing goes to the healthy tissue instead of the tumor and causes damage there. To prevent this, each patient's vascular structure is examined by performing a rehearsal angiography before the treatment. It is observed whether there is any leakage outside the liver. The doses and amounts of radiation each patient will receive are different. The angiography of each patient is different. Each of these is calculated according to detailed calculations and an evaluation is made for the patient. Afterwards, the radioactive substances calculated as in the rehearsal are injected using the same method. "After the injection, PET images are taken to review whether the administered substance reaches the correct target or whether the patient will benefit from this treatment."
Can the Patient Be Discharged Immediately After RadioEmbolization Treatment?
Interventional Radiology Specialist Assoc. Prof. Dr. Melih TOPÇUOĞLU said that after the procedure, the patient was discharged on the same day or the next day. Dr. TOPÇUOĞLU stated that the response of cancerous tissues to this treatment is expected at the earliest between the 6th, 9th and 12th weeks. Dr. TOPÇUOĞLU reminded that controls were achieved with MRI and PET CT imaging approximately 3 months later. Dr. TOPÇUOĞLU said that it is possible to give patients a second chance for treatment depending on the size of the metastases or liver tumor. Dr. TOPÇUOĞLU said, “Patients who have been rehearsed for the first session angiography come to the interventional radiology unit for the actual treatment. When they arrive we perform angiography as a standard through the needle hole in the right groin and rarely in the wrist. The aim here is to inject structures called microspheres, which contain pre-calculated and loaded radioactive material, into cancerous tissues through the arteries that feed the cancer. We perform this procedure, which is very comfortable for the patient with local anesthesia. This process takes approximately 30 minutes to -90 minutes, depending on experience. Since the artery map of the cancerous tissue is created during the rehearsal process, which is the first angiography session, the second angiography always takes much shorter. "Since the patients become familiar with how the procedure is performed during the rehearsal angiography, the second session of treatment angiography becomes much more comfortable," he said.
This content was prepared by Yeditepe University Hospitals Medical Editorial Board.
”
See Also
- Diagnosis of Heart and Brain Diseases with PET CT
- Atomic Therapy (Radioactive Iodine Therapy)
- Therapies Applied in Nuclear Medicine
- Theragnostic Approach in Cancer Treatment
- Nuclear Medicine Diagnosis and Imaging
- Diagnosis and Treatment of Acute Stroke
- The Cause of Abdominal Pain Has Not Been Found for Years... Varicose Veins Appeared in Her Ovary
- Interventional Methods in the Treatment of Acute Stroke
- Interventional Radiology is Used in Many Fields
- What Diseases Is Interventional Radiology Used For?
- Molecular Imaging and Treatment in Prostate Cancer
- Lutetium Treatment in Neuroendocrine Tumors
- What is a Brain Aneurysm?
- Targeted Atomic Therapy is Hope for Many Cancers
Alo Yeditepe