Alo Yeditepe
Alo Yeditepe
Obesity Surgery
At Yeditepe University Hospital's Bariatric Surgery Clinic, after identifying the causes of the patient's obesity, patients are evaluated by a coordinated team consisting of a surgeon experienced in the field, an endocrinologist, and a nutrition and diet specialist. In this system, known as a multidisciplinary approach, specialists in Bariatric Surgery, Endocrinology and Metabolic Diseases, Nutrition and Dietetics, Physical Therapy and Rehabilitation, and Psychology evaluate the patient and shape the treatment process.
In addition, the necessary equipment, including advanced technologies, and intensive care facilities are available.
What is Obesity?
"Obesity is defined as having more than a certain amount of fat in the body. This ratio is determined by a calculation that includes our height and weight. This is called the body mass index (BMI). However, body type and the amount of muscle in the body are also taken into account when defining obesity.
If the body mass index is above 40 kg/m2, it can be said that the person is at a level of weight that is considered a disease. This condition is also defined as morbid obesity. Individuals with a BMI (body mass index) value above 35 who also have additional weight-related conditions such as type 2 diabetes, heart disease, hypertension, and sleep apnea are considered obese patients requiring treatment.
It is now widely accepted that obesity contributes to diseases that shorten human life expectancy. Obesity is known to increase the risk of conditions such as diabetes, high blood pressure, sleep apnea, heart and vascular diseases, hyperlipidemia, fatty liver disease, kidney disease, and joint disorders, as well as increasing the incidence of certain types of cancer.
What is Obesity Surgery, Why and When is it Necessary?
Bariatric surgery, also known as obesity surgery, is the collective name for surgical procedures that enable obese patients to lose weight by making changes to the digestive system. Today, the most effective treatment for obesity is provided through surgical methods. In the treatment of many diseases, patients are advised to lose weight to extend their lives and improve their quality of life, which is negatively affected by obesity-related diseases.
The healthiest way to lose weight is through changes in diet and physical activity. If patients are unable to lose weight despite these efforts, they are evaluated for obesity surgery. A decision on whether patients are suitable candidates for surgery is made based on the assessments of specialists from the endocrinology, psychiatry, chest diseases, internal medicine, and cardiology departments.
Who is Eligible for Obesity Surgery?
Patients with a body mass index (BMI) over 40 kg/m² and obesity-related diseases, or patients with a BMI over 35 kg/m² who have tried numerous other weight loss methods without success, are considered for surgical treatment. Depending on the patient's clinical characteristics and performance, patients between the ages of 18 and 65 are candidates for surgery if they will continue clinical follow-ups, comply with post-operative recommendations, do not have major psychiatric illnesses, are not substance abusers, and do not have underlying medically treatable diseases that cause obesity.
What Are the Benefits of Obesity Surgery for the Patient?
"Bariatric surgery is much more successful than other treatment methods in promoting weight loss. Although a reduction in food intake and restricted nutrient absorption are the main factors, differences in the hormones that regulate hunger and satiety also contribute to weight loss by reducing hunger and overeating. In addition, it becomes easier for the person to adapt to the changes they need to make in their diet. The number and type of bacteria in the intestine change after obesity surgery. Therefore, the bacterial metabolites involved in the gut-brain axis show beneficial changes. Social and psychological confidence makes it easier to resist the urge to overeat.
Following bariatric surgery, the treatment of obesity reduces the risk of many health problems such as type 2 diabetes, cardiovascular disease, hypertension, neurological disorders, sleep apnea, kidney disease, joint disease, and fatty liver disease.
In addition, weight control achieved after obesity surgery reduces the incidence of many cancers, such as colon cancer, uterine cancer, and colorectal cancer. Being at a healthier weight contributes to an improved quality of life. The reduction in problems associated with additional diseases also has a positive effect on life expectancy.
Why is Obesity Surgery More Effective than All Other Treatments?
In obesity treatment, diet and physical activity are the healthiest methods if success can be achieved. However, even the best results in morbidly obese patients have not exceeded 5% success. Obesity surgeries limit the amount of food consumed by reducing the size of the stomach. In addition, although the feeling of hunger is not the same in every patient, it enters a one-year honeymoon period and decreases. It becomes easier for the patient to adapt to a weight-loss diet. Eating habits are one of the most important problems in obesity, and the patient's eating behavior changes after surgery. Changes in certain hormones in the small intestine and the nervous system also help the patient lose weight. Changes in the intestinal microflora after bypass surgery contribute to weight loss.

Obezite Cerrahisi Diğer Tüm Tedavilerden Neden Daha Etkilidir?
Obezite tedavisinde, eğer başarı yakalanabilirse en sağlıklı yöntem diyet ve fiziksel aktivitedir. Ancak morbid obez hastalarda en iyi sonuçlar bile %5’in üzerinde başarıya ulaşmamıştır. Obezite ameliyatları midenin küçülmesi ile birlikte alınan besin miktarını sınırlar. Bunun yanında açlık hissi her hastada aynı olmamakla birlikte bir yıllık bir balayı dönemine girer ve azalır. Hastanın kilo verici beslenme düzenine uyum sağlaması kolaylaşır. Yeme alışkanlıkları obezitenin en önemli sorunlarından biridir ve cerrahi sonrası hastanın beslenme davranışları değişir. İnce barsaktaki bazı hormonlarda oluşan değişiklikler ile sinir sisteminin de hastanın kilo vermesine yardımcı olması sağlanır. Bypass ameliyatları sonrasında barsak mikroflorasındaki değişiklikler kilo verilmesine katkıda bulunur.
Who is not a Suitable Candidate for Obesity Surgery?
The decision to undergo bariatric surgery is made by the doctor based on many criteria, such as the patient's general health, psychological state, and potential for post-operative compliance.
In addition, bariatric surgery is generally not recommended in the following cases:
People with serious heart, lung, or liver disease.
• Individuals with uncontrolled psychiatric disorders. Individuals whose illnesses are under control may also be evaluated.
• Individuals with alcohol or substance addiction.
• Individuals who have gained weight due to hormonal disorders but whose disorders have not been treated.
• Individuals who are not thought to be able to adapt to lifestyle and dietary changes after surgery.
What Are the Risks of Obesity Surgery?
Bariatric surgeries are major surgical procedures and, like any surgery, carry their own risks. However, bariatric surgeries are now performed with high success rates.
You can find detailed information about the risks of bariatric surgery here.
What Diseases Does Obesity Cause?
Obesity is recognized as a global problem that is becoming increasingly widespread throughout the world today. It is considered a disease in itself and is also significant in terms of being a risk factor for many chronic diseases.
Some of the diseases for which obesity is a risk factor can be listed as follows:
• Type 2 diabetes
• High blood pressure (hypertension)
• Cardiovascular diseases such as coronary artery disease and heart failure
• Risk of vascular occlusion and stroke
• Sleep apnea and respiratory problems
• Fatty liver (non-alcoholic steatohepatitis)
• Joint and muscle problems, especially in the knees and hips
• Certain types of cancer, such as colon, breast, and kidney cancer.
What are the methods of Obesity Surgery?
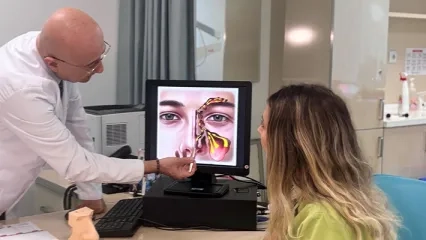
Obesity surgeries can be restrictive, reducing the volume of the stomach, or restrictive and malabsorptive, aiming to both reduce the volume of the stomach and decrease food and calorie intake. The decision on which surgery to perform is made after a detailed discussion of the patient's body mass index, evaluation of additional diseases, success rates, and risks.
You can find information about bariatric surgery methods here.

Frequently Asked Questions About Bariatric Surgery
Is There an Age Limit for Obesity Surgery?
Of course, there is an age limit for bariatric surgery. The ideal age for bariatric surgery is considered to be between 18 and 65. However, the patient's overall condition is very important at this point. For example, in young people aged 16-18, surgery may be planned with a special evaluation if there is severe obesity and accompanying health problems. However, this is an exceptional situation and must be evaluated by a physician.
In addition, the decisive criterion for the upper age limit is the patient's general health. The decision to perform bariatric surgery is made by evaluating underlying chronic diseases.
How Should Nutrition Be Managed After Obesity Surgery?
Proper nutrition after bariatric surgery supports both healthy weight loss and the success of the surgery. Therefore, following a nutrition plan created in accordance with the recommendations of a specialist dietitian after bariatric surgery is the most appropriate method.
In general, after bariatric surgery, it is necessary to consume plenty of water, eat slowly, and avoid excessive sugar and fat.
Is Bariatric Surgery Dangerous?
Bariatric surgeries are major surgical procedures and, like any surgery, carry their own risks. However, bariatric surgeries are now performed with high success rates.
You can find detailed information about the risks of bariatric surgery here.
When Can I Exercise After Obesity Surgery?
At the end of the first week, the patient will return to their daily life. They can engage in light walking activities. Before starting sports and exercise after obesity surgery, the body's healing process should be taken into account, and action should only be taken with the doctor's approval. If everything goes well after surgery, the patient can return to their daily life after the first week. Light walks are generally recommended for the first 2-3 weeks. Aerobic activities and swimming can be started at the end of the first month, while strenuous resistance exercises can be done after two months.
However, you should remember that your doctor will make the final decision on this matter and that you should act according to their recommendations.
”
See Also
- Revision Surgery in Obesity Surgeons
- Swallowable Gastric Balloon
- They Set Out Together For Their Dreams
- What are the Types of Obesity Surgeries?
- Questions About Obesity Surgery
- A New Era in Obesity Surgery
- Overweight
- Due to His Weight, He Could Not Take Care of His Children; He Lost 57 Kilograms and Regained His Health
- Are Obesity Surgeries Risky?
Alo Yeditepe